Abstract
Introduction: While most patients with mantle cell lymphoma (MCL) receive therapy shortly after diagnosis, a subset of patients with indolent-behaving disease can safely defer treatment (Calzada et al, 2018). In this subgroup, a lack of evidence to support the decision-making behind the choice of therapy has led to a wide diversity in treatments. We evaluated the importance of treatment intensity in patients with MCL who defer initial therapy.
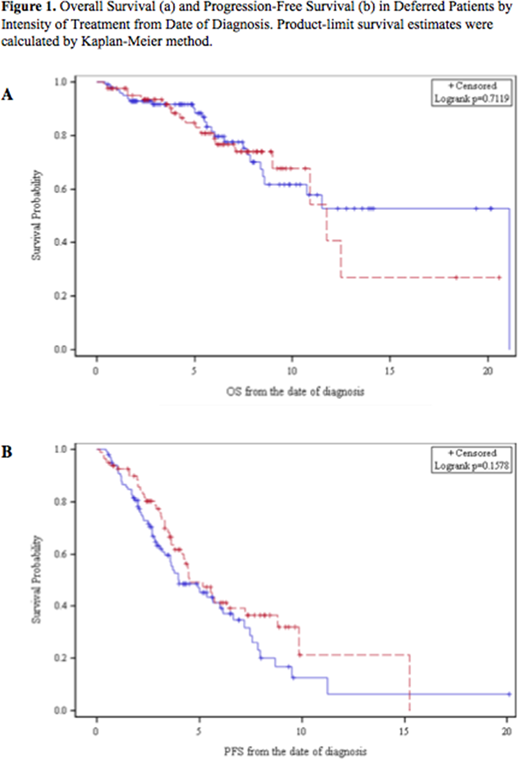
Methods: We included patients ≥ 18 years old with MCL from 11 academic centers and defined the deferred subgroup as patients who started therapy ≥ 90 days after diagnosis. Patients who received high dose cytarabine as part of their induction or autologous stem cell transplantation (ASCT) in first remission were considered to have received intensive therapy while all other approaches were non-intensive. We identified differences between the baseline characteristics of the two groups using Fisher's exact tests, chi-squared tests, and t-tests as appropriate. We calculated progression-free (PFS) and overall survival (OS) from the date of diagnosis using the Kaplan-Meier method and compared the two groups using the log-rank test. Univariate and multivariate Cox proportional hazards models were performed for PFS and OS.
Results: Of 968 identified patients with MCL, 233 did not initiate therapy within 90 days of diagnosis and were considered deferred. Deferred patients had a lower Ann Arbor stage (p<0.001), Ki-67 (p<0.001) and LDH (p=0.007) at diagnosis compared to patients undergoing immediate treatment. Within the deferred group, 80 patients received intensive therapy (including 59 who completed ASCT in first remission), 99 received non-intensive therapy, and the remaining 54 patients did not receive any documented treatment and were excluded from this analysis. The most common intensive regimens included R-HyperCVAD and R-CHOP, and the most common non-intensive regimens included R-bendamustine and R-CHOP without ASCT. There was no difference in time to treatment, ECOG performance status, ethnicity, Ann Arbor stage or presence of B-symptoms between the two groups. However, patients who received non-intensive therapy were older (p<0.001), more likely to have a normal LDH (p=0.03), and more likely to be treated at the reporting academic center (p=0.008).
There was no significant difference in OS (Figure 1A, p=0.7) or PFS (Figure 1B, p=0.16) between the deferred patients who subsequently received non-intensive vs. intensive therapy. Univariate analysis of PFS highlighted the significance of: LDH (HR 0.62, p= 0.04), lack of blastoid morphology (HR 0.53, p=0.032), treatment initiation at participating academic center (HR 0.43, p<0.001), post-induction rituximab (HR 0.42, p=0.003), and higher baseline hemoglobin level (HR 0.90, p=0.038) as predictors of improved PFS. Multivariable analysis demonstrated that post-induction rituximab (HR 0.16, p=0.008) and treatment initiation at an academic center (HR= 0.17, p<0.001) predicted improved PFS while pre-existing coronary artery disease (HR=5.28, p=0.015) was associated with decreased PFS.
A univariate analysis found that lack of blastoid histology (HR 0.24, p<0.001), normal LDH (HR 0.31, p<0.001), increased baseline hemoglobin (HR 0.83, p=0.005), post-induction rituximab (HR 0.16, p=0.014), and treatment initiation at an academic center (HR 0.34, p=0.003) significantly improved OS. In a multiviariable analysis, lack of blastoid histology (HR 0.11, p<0.001) predicted improved OS while pre-existing diabetes mellitus (HR 5.98, p=0.005) and age (HR 1.08, p=0.001) were significantly associated with inferior OS. Intensity of treatment was not significantly associated with PFS or OS in the univariate or multivariable models.
Conclusions: Among this large group of MCL patients who deferred therapy, use of an intensive induction therapy did not improve OS or PFS compared to patients who received non-intensive treatments. Our findings suggest that other patient- and disease-related factors may affect PFS and OS in this patient subgroup. Prospective studies to evaluate tools incorporating these factors will be useful in identifying the optimal therapy approach for patients with MCL who have completed an initial period of observation.
Calzada:Seattle Genetics: Research Funding. Bachanova:Kite Pharma: Membership on an entity's Board of Directors or advisory committees; GT Biopharma: Research Funding; Gamida Cell: Research Funding. Barta:Janssen: Membership on an entity's Board of Directors or advisory committees; Merck, Takeda, Celgene, Seattle Genetics, Bayer: Research Funding. Danilov:Takeda Oncology: Research Funding; Gilead Sciences: Consultancy, Research Funding; Genentech: Consultancy, Research Funding; Astra Zeneca: Consultancy; TG Therapeutics: Consultancy; Verastem: Consultancy, Research Funding; Aptose Biosciences: Research Funding; Bayer Oncology: Consultancy, Research Funding. Grover:Seattle Genetics: Consultancy. Karmali:Gilead: Speakers Bureau; AstraZeneca: Speakers Bureau. Hill:Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Research Funding; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Seattle Genetics: Honoraria, Membership on an entity's Board of Directors or advisory committees; Seattle Genetics: Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Genentech: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Honoraria, Membership on an entity's Board of Directors or advisory committees. Park:Rafael Pharma: Consultancy; BMS: Research Funding; Seattle Genetics: Research Funding; Seattle Genetics: Speakers Bureau; BMS: Consultancy; Teva: Research Funding; Gilead: Speakers Bureau; Takeda: Research Funding; G1 Therapeutics: Consultancy; Teva: Consultancy. Blum:Novartis: Research Funding; Seattle Genetics: Research Funding; Celgene: Research Funding; Morphosys: Research Funding. Hamadani:Cellerant: Consultancy; Celgene Corporation: Consultancy; MedImmune: Consultancy, Research Funding; Sanofi Genzyme: Research Funding, Speakers Bureau; Ostuka: Research Funding; Takeda: Research Funding; ADC Therapeutics: Research Funding; Merck: Research Funding; Janssen: Consultancy. Kahl:Genentech: Consultancy; Seattle Genetics: Consultancy; ADC Therapeutics: Research Funding. Flowers:Denovo Biopharma: Consultancy; Celgene: Research Funding; Spectrum: Consultancy; Eastern Cooperative Oncology Group: Research Funding; Gilead: Research Funding; Pharmacyclics/ Janssen: Consultancy; BeiGene: Research Funding; Bayer: Consultancy; Pharmacyclics: Research Funding; TG Therapeutics: Research Funding; Burroughs Wellcome Fund: Research Funding; V Foundation: Research Funding; Abbvie: Research Funding; Gilead: Consultancy; Janssen Pharmaceutical: Research Funding; OptumRx: Consultancy; Genentech/Roche: Consultancy; Millennium/Takeda: Research Funding; Abbvie: Consultancy, Research Funding; Karyopharm: Consultancy; National Cancer Institute: Research Funding; Genentech/Roche: Research Funding; Acerta: Research Funding. Cohen:Bristol-Myers Squibb: Research Funding; Bristol-Myers Squibb: Research Funding; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Infinity Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees; AbbVie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees; AbbVie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Research Funding; Infinity Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Research Funding; Millennium: Consultancy, Membership on an entity's Board of Directors or advisory committees; Millennium: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pharmacyclics: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Research Funding; Takeda: Research Funding; BioInvent: Consultancy; BioInvent: Consultancy; Seattle Genetics: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Seattle Genetics: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal